The Public Health Emergency Propping Up Telehealth
A COVID-19 telehealth policy measure was just extended by Congress through 2024
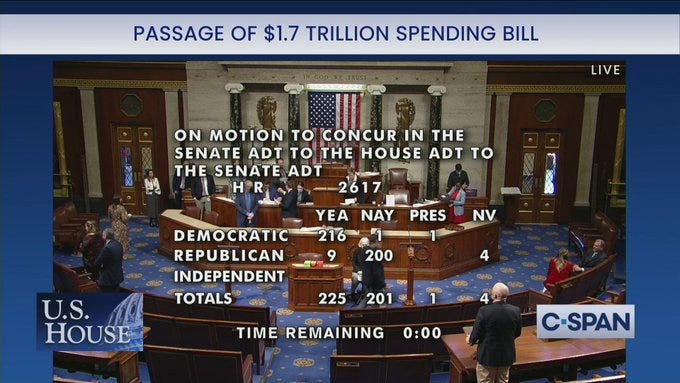
Among the numerous provisions of the last spending bill passed by the 2022 Congress was an extension of flexibilities in telehealth laws that began with the COVID-19 pandemic public health emergency. Being approved through 2024, these exceptions have now outlived the public health emergency which allowed them to take shape. So what exactly did Congress just approve? What does that mean for remote healthcare options in the country?
Public Health Emergencies
The US federal government has a partnership between the Departments of Health and Human Services (HHS), Veterans Affairs (VA), and Defense (DoD) called the National Disaster Medical System (NDMS).
This partnership can provide medical and healthcare support services in response to public health emergencies (PHE’s), offering support to state, local, tribal, and territorial teams on the ground. For military health emergencies, NDMS also has the authority to assist the military and VA in treating combat casualties.
When the Secretary of HHS or President declares a PHE, the NDMS activates and unleashes vast resources which have historically been used for crises including but not limited to:
hurricanes
tornado outbreaks
wildflowers
opioid crisis
Most notably for today’s discussion, PHE’s have also been declared for disease outbreaks like H1N1, Zika, and COVID-19. By default, these PHE’s last up to 90 days but can be extended by the Secretary.
The Secretary of HHS gains new powers under Section 319 of the Public Health Service Act (PHS). They can, among other actions:
create grants and initiate contracts for conducting and supporting investigations
access parts of the Public Health Emergency Fund
allow the Centers for Disease Control and Prevention (CDC) director to access Infectious Diseases Rapid Response Reserve Fund
grant extensions and flexibilities on data that must be reported
allow the DoD to deploy military trauma care providers
Basically, HHS can tap into rainy day funds immediately without having to wait for Congress to get more cash while bypassing traditional operating procedures.
Note that HHS also runs large programs like Social Security, Medicare, Medicaid, and the Children’s Health Insurance Program (CHIP). In the event of a PHE, section 1135 of the Social Security Act lets HHS waive and modify requirements for these programs.
1135 Waivers and Telehealth
HHS’ 1135 waivers are intended to allow the Department to sidestep laws and regulations that would otherwise impede the delivery of emergency healthcare services. To help care providers see more patients in the face of limited space at healthcare facilities, HHS waived rules that limited telehealth services.
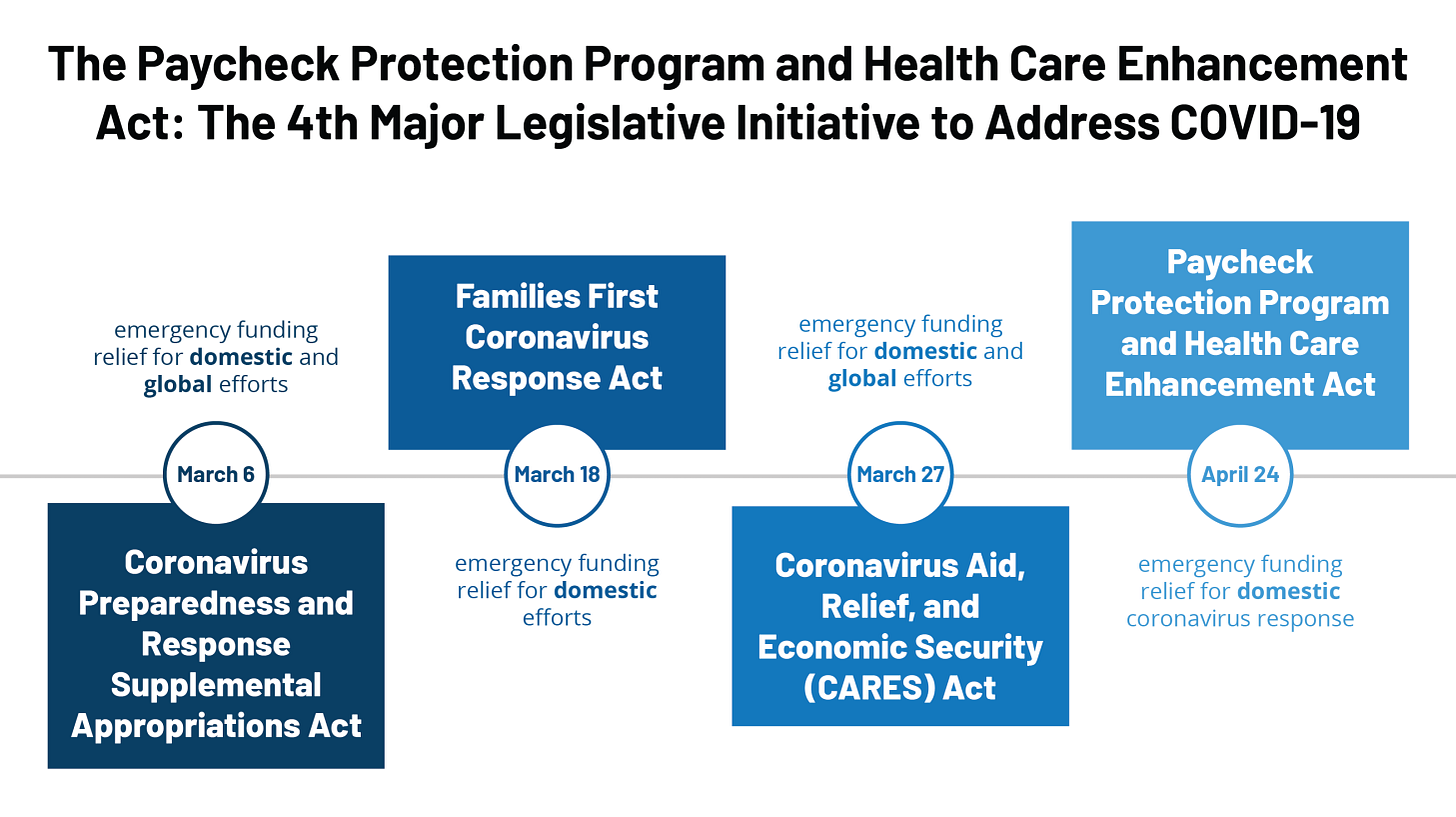
In fact, these changes were so extensive, that 1135 wavier powers had to be broadened by the Coronavirus Aid, Relief, and Economic Security Act (CARES Act).
Prior to the public health emergency, the Centers for Medicare and Medicaid Services (CMS) imposed restrictions on which services doctors could administer remotely and bill Medicare for. Because Medicare is a significant revenue stream for many providers seeing older patients, and because certain services could not be billed if administered remotely, there were many medical services that doctors would not offer via telehealth.
The CARES Act gave CMS the authority to waive these limitations on what services could be billed for when given to the patient via telehealth. All of a sudden, there was a revenue potential for giving these services remotely. Combined with another waiver allowing providers to bill Medicare for services furnished with audio-only telehealth options, this 1135 waiver unleashed a wave of new telehealth offerings.
The number of CMS beneficiaries has grown from 12,000 weekly telehealth visits to "well into six figures"
Source: Becker’s Hospital Review June 2020
Extensions and Tough Questions
These telehealth waivers are set to end 151 days after the end of the COVID-19 PHE. The COVID-19 PHE is currently set to expire today, but the spending bill passed by the outgoing 2021-2022 Congress overrode the 151-day post-PHE expiration of the telehealth flexibilities. Now, these flexibilities will stay through 2024.
So what’s going to happen after 2024?
The American Hospital Association, a lobbying group representing hospitals, endorses continued extension of these telehealth flexibilities. Why wouldn’t they? Telehealth services are cheaper to administer, because now you can see more patients with less overhead from running an in-person facility.
There are of course arguments that such telehealth flexibilities give providers a financial incentive to maintain support of remote offerings that open the door to better accessibility of medical services to rural populations that otherwise face high barriers to visiting medical facilities in-person.
However, telehealth come with a host of vulnerabilities related to secure exchange of patient health information. Such expansion of telehealth usage must come with safeguards to protect patient privacy. Because Medicare is funded by the taxpayer, there are also necessary discussions about whether healthcare professionals should be paid the same for giving in-person and telehealth services. In the event that telehealth services are compensated less by Uncle Sam, how do we make sure that providers don’t make the business decision to offer less telehealth services which yield lower revenue?
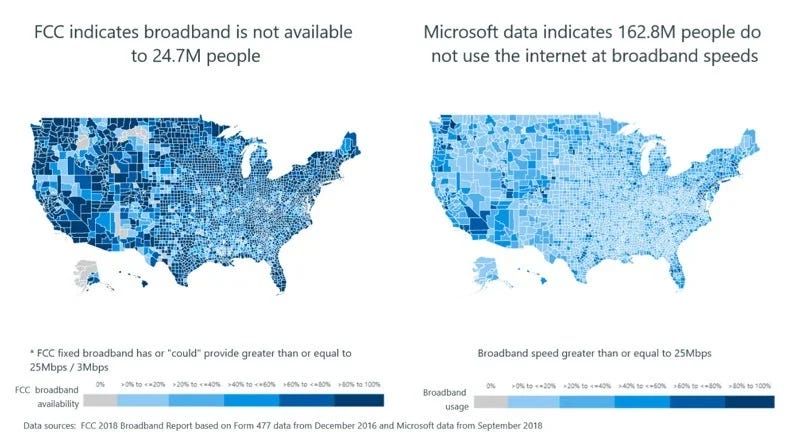
Then of course, what do we do about populations with limited access to broadband technology and poor digital literacy? Before wholly committing to telehealth, the federal government must put forward plans to ensure disadvantaged communities don’t get left too far behind by a national commitment to telehealth.